Every programme delivered by NAPC starts with asking what it means for the health and well-being of the population and the sustainable delivery of care and support. This is nowhere more evident than in the CARE programme, supported by NHS England and delivered by the National Association of Primary Care (NAPC).
CARE is a learning and development programme that empowers and activates primary health and care professionals to lead change within their practice, primary care network or neighbourhood. The programme equips individuals through training and support to look at their approach including personal impact, their leadership skills and the application of population health improvement approaches to develop or change local services with a measurable difference.
The CARE programme is for all staff committed to making positive changes to benefit both their colleagues and all those who require health and care services. The programme is delivered over 8 modules, each module designed to build the understanding, skills and application of:
- An increased understanding and application of population health improvement
- Developing leadership for system impact
- Building personal resilience and wellbeing
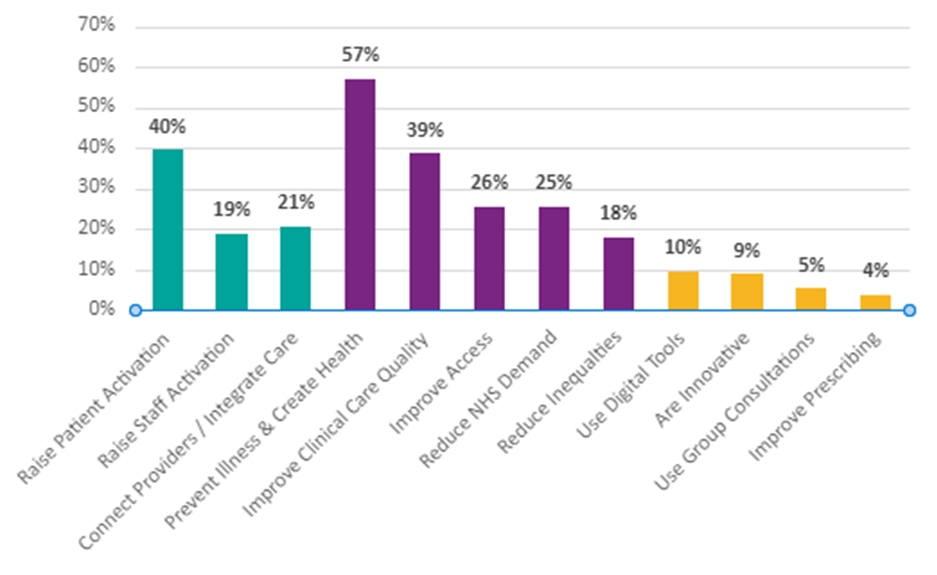
600+ projects have been grouped into 12 impact areas
Through working with over 700 staff on the programme we have recognised the value and impact of patient and staff activation as a pivotal measure for change and impact.
Patient activation is a widely recognised concept and describes the knowledge, skills and confidence a person has in managing their own health and well- being. Staff activation encourages members of the team to authentically engage, to take control and begin to innovate and share content about topics that interest them that benefit themselves, their team members and also the patients that they serve. When staff are activated, they respond by innovating and scaling those innovations while encouraging others to do the same and when patients are activated, they don’t just maintain their health and wellbeing they improve it themselves and spur others to do the same.
And when activated staff or patients are activating others, that snowball effect is a self-reinforcing behavioural shift.
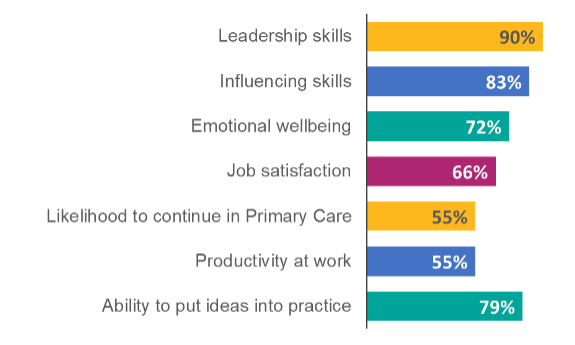
Originally aimed at General Practice Nurses, CARE has been expanded to include the wider primary and community care team, including pharmacists, physiotherapists, paramedics, practice managers, health and wellbeing coaches, GPs and all roles within community and social care. demonstrating an approach that underpins the grassroots change needed to support real integrated working. NAPC is delivering the programme across England, working with 41 of the 42 systems and the table below outlines the improvements across a range of factors:
The Innovations
CARE has supported over 600 projects aimed at:
- Activating Patients: Over 70% of diabetes projects take a multidisciplinary approach to support patients in self-management and to facilitate lifestyle changes.
- Addressing Inequality: Approximately 25% of projects strive to bridge health inequities by connecting underserved populations with healthcare and community resources.
- Digital Engagement: A significant number of projects utilise text nudges, digital tools, and virtual group consultations to provide support more efficiently.
- Clinical Care Protocols: Several initiatives focus on developing standardised care protocols and optimising medication for diabetes management.
Additionally, those that have been through, or are existing participants on the programme have evidence of significant improvements across the programmes they have been supported to deliver that benefit not just the patient, but other practitioners in their team and in many cases themselves too. One programme that focussed on diabetes care significantly reduced the GP workload (as demonstrated below) through the implementation of simple interventions such as introducing personal text messaging to patients. By taking this approach the relationship with the nurse specialist or GP is not lost.
Innovations include:
- Text Nudges: Text support reduced diabetic HbA1c by 9 mmol/mol between reviews.
- Group Support: Virtual care and goal-setting cut HbA1c by 28% and BMI by 4%.
- Telephone Outreach: Calls to disengaged patients reduced GP contacts by 7 annually, improving HbA1c and BMI.
Evaluation of the programme and the various innovations that have been implemented show that when activation improves, it’s only a matter of time before physical health improves and GP contacts fall.
A 1-point rise in activation is correlated to a saving of up to 5 GP contacts per patient per year and a 1-point rise in activation is correlated to primary and secondary care demand savings of £327 per patient per year.
When it comes to staff wellbeing, one practice nurse looked at the impact of breaks on
performance. Unsurprisingly, the results demonstrated an 8% improvement in work performance, so missing breaks because of workload isn’t just bad for staff health and wellbeing but can also leads to increases in short term demand pressure via reduced productivity.
We know that patients with multiple Long-Term Conditions (LTCs) often struggle to attend annual reviews and the clinical focus can lead to unmet needs and duplication of work.
One practice nurse set up personalised multimorbidity reviews, consolidating all LTCs into one appointment. She set up a triage process to provide longer reviews for patients with poor control or greater risk and shorter appointments for well-managed patients. She also utilised new roles, such as care coordination and social prescribing, to tailor support, address underlying needs and reduce GP workload.
She continues to develop in her own role while rolling out this model across other PCNs. The results yielded so far include: 44% increase in patients attending reviews, fewer appointments, enhanced self-management and improved health outcomes and across the system a 2% reduction (856 hours annually) in total GP demand estimated and decreased duplication of work like blood tests.
One of the course participants told us:
“I started my nursing career in acute care and have held senior roles in paediatric wards and A&E. I took a career break to have my children and returned to nursing at a GP practice. I am lead nurse at my surgery which has a patient population of 20,000. I’m also lead nurse for a PCN. Although I’ve held senior roles for a number of years, I’ve never had any formal leadership training. It’s often difficult to access learning that really targets the needs of nurses in primary care, so I was very pleased when the opportunity to take part in the CARE programme came along.
“As nurses we aim to be the best we can be, and I saw taking part in the CARE programme as an opportunity to discover a little more about myself and to delve more deeply into what makes a good leader. I also wanted to network, develop relationships and share ideas with other clinicians in my health system. I liked the idea of working towards similar goals in a supportive environment.
“The programme has opened up new ways of thinking about care delivery and improving patient outcomes. For example, we have explored population health management and the use of data to make improvements to services. We also worked through useful and practical concepts and tools such as Six Thinking Hats and Nancy Kline’s Thinking Environment. The programme’s focus on population health management, its high-quality content and opportunities to network and learn from others has been invaluable.”
“Never doubt that a small group of thoughtful committed individuals can change the world. In fact, it’s the only thing that ever has.”
Margaret Mead, American cultural anthropologist

